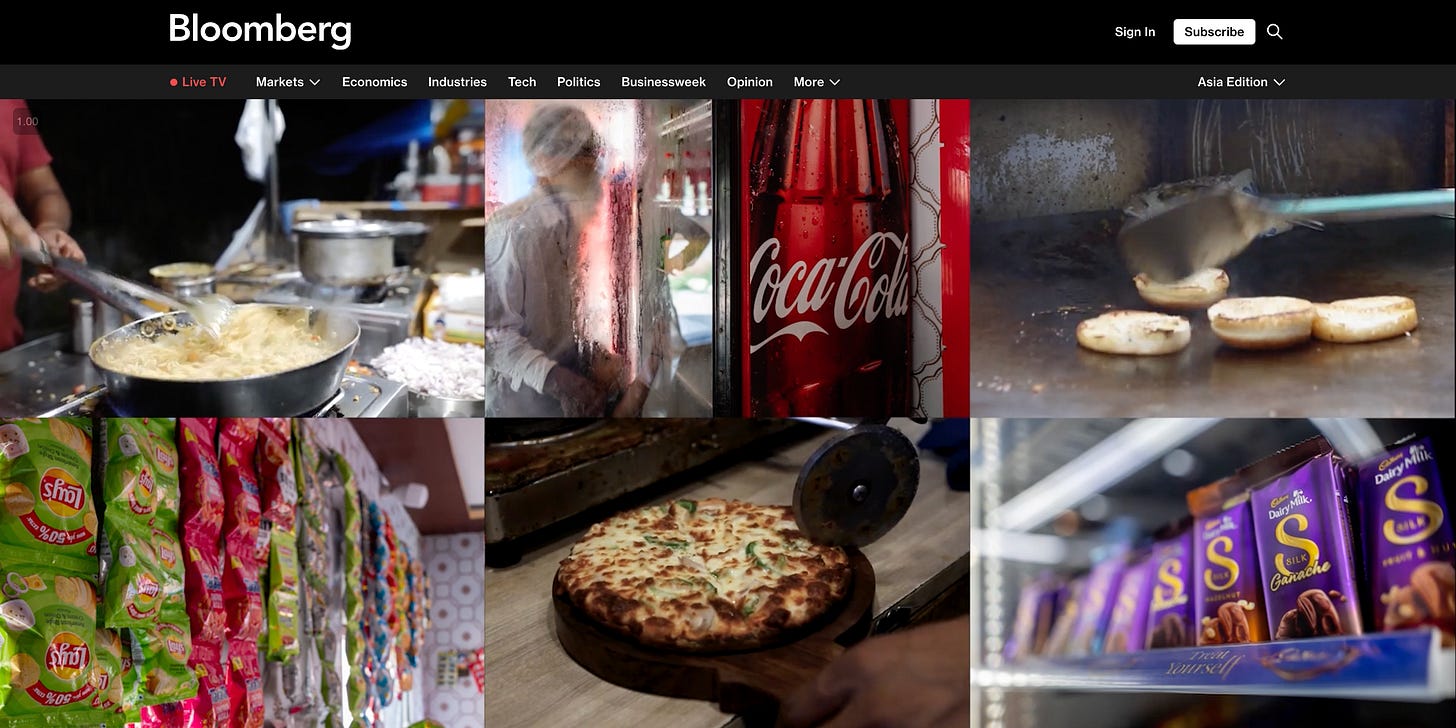
Obesity in India — Big Food's "fantastic growth engine"
India's obesity rate has tripled over the past 30 years. Is there any hope?
Recently, India overtook China as the most populous country, with an eye-popping 1.4 billion people. With these numbers, any healthcare system would struggle to cope, but one of India’s most existential threats is obesity. After all, this disease is linked with 224 complications, from high blood pressure to diabetes to over a dozen types of cancers, and India has the third steepest obesity rates in the world. The adult obesity rate, meanwhile, has tripled over the past 30 years.
Bloomberg has a terrific feature on India’s obesity crisis, so you should read that here. But in this short newsletter, I’ll summarize some of their reporting and offer my own reflections, after speaking with senior citizens in New Delhi’s slums and shadowing a bariatric surgeon in the city’s Max Super Specialty Hospital.
While the solution to obesity is often-wrongly assumed to be diet and exercise alone, it’s true that they contribute to obesity onset, as well as the larger “obesogenic” environment. In recent years, Western countries have pushed greater regulation and awareness campaigns about ultra-processed foods, while anti-obesity drugs like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) seem like they’re changing food purchasing. Given such headwinds, the packaged food and beverage industry has looked globally to find new markets, with India one of its most promising “lifelines.” Bloomberg reports:
“Countries like Mexico, where childhood obesity is a leading health concern, have restricted companies from advertising unhealthy food to youth. But no such rules exist in India. Starchy cereals and sugary drinks are sold as quality options in commercials featuring Bollywood actors and cartoon characters.”
Bloomberg then offers the example of Unilever, an industry giant that anticipates India will drive the company’s revenue within ten years: “‘India’s on fire,’ said Hanneke Faber, the outgoing head of nutrition at Unilever, calling the country a ‘fantastic growth engine.’”
It’s a sobering assessment but also a well-established one: the tobacco industry similarly shifted to emerging markets after Western countries started to regulate their products. A little-known fact is that, in the 1980s, tobacco industry giants bought up processed food companies as part of their diversification schemes. Who better to know how to make something addictive?
Dealing with obesity in India is difficult, given the dual challenges of overnutrition and undernutrition, according to Monika Arora, Vice President or Research and Health Promotion at the Public Health Foundation of India. For a country that has predominately struggled with malnutrition alone, this shift is testing the government’s ability to respond and underlining the need to strengthen the healthcare system.
One critical part of any response is treatment, the gold-standards of which include intensive behavioral therapy, medications, and bariatric surgery — where surgeons reduce the size of the stomach and bypass some of the small intestine. This not only restricts the food a patient can eat but also shifts their hormones in a healthier direction — since the stomach, intestines, and fat cells make certain appetite and hunger-promoting hormones. I wanted to learn more about this procedure, so I met with Dr. Manish Baijal, a laparoscopic and bariatric surgeon at Max Super Specialty Hospital, to observe his operations and learn about how he’s thinking about the rising tide of obesity in India.
The morning started with a sleeve gastrectomy case on a woman with BMI of 45 (obesity is defined as BMI≥25 in India). The operation was done minimally invasively, meaning that the surgeons made four small incisions in the women’s belly — three for putting surgical instruments and one for the camera — before inflating the belly with CO2 to create room to maneuver. For the next 60 minutes, the surgeons then watched a monitor, as they snipped, cauterized, and dug their way through the patient’s abdomen. Have you ever typed without looking at your keyboard? It’s a little like that, except a “typo” here could be fatal.
Still, this operation is relatively simple. Dr. Baijal first worked his way to the patient’s stomach, separating it from surrounding structures and pulling back the greater omentum — a large fatty structure, which drapes over the abdominal organs. (It looks a little like the yellow spongy insulation you might find in your walls.) Then, the surgical team placed a “bougie,” or small sizing tube, through the patients’ mouth down into their stomach — to determine how small to make the stomach.
After all this preparation, Dr. Baijal cut out roughly 75% of the stomach, using a stapler across the organ so that this “sleeve” left behind would restrict food intake. (The surgical team confirmed it by filling the patients’ stomach with saline and blue dye to make sure nothing seeped out of the staple line.) Finally, Dr. Baijal removed the excised stomach from the patient’s body — by placing it into a specimen bag, pulverizing the contents into smaller bits, and then pulling the bag out one of the small abdominal incisions. After that, it was just a matter of closing up and waking up the patient.
“The problem in India is bariatric surgery acceptance is very poor,” says Baijal, after we returned to his office post-operation. The patients who come to him have “tried every possible thing at some point of time” yet often are still “scared of surgery, that they can die,” Baijal says. “They feel with obesity, at least they are living. But it is only temporary; they don’t understand that the risk of dying with obesity is so high.” The other challenge with bariatric surgery is that it’s quite expensive. And outside the crowded public system with their infamous waiting lists, patients have to pay out of pocket — about $4000-7000 at Max.
It doesn’t help that Baijal’s fellow doctors have similarly limited awareness and knowledge of bariatric surgery. He’ll see patients sitting outside the endocrinologist’s outpatient clinic with relatively high BMIs, “and they would never be advised for surgery,” even if eligible and very likely to benefit. The data show that bariatric surgery is the most effective treatment for severe obesity, helping patients lose about half of their excess weight, while curing hypertension, sleep apnea, and diabetes in 62%, 77%, and 86% of patients. The mortality rate, in turn, is about 0.5% — pretty low, all things considered.
If India is ever going to truly address obesity, it’s clear that bariatric surgery will be a big part of the solution. But that might require a revolution in public opinion.
During my reporting, what surprised me most was that there is some emerging evidence on a reversal of the socioeconomic gradient in India when it comes to obesity, according to Arora. Namely, obesity is thought to be a disease of the wealthy in low- and middle-income countries (LMICs); after all, they have the money to eat well and avoid physical labor. But increasingly, Indians in urban slums are developing obesity, Arora says, with little money to buy fruits and vegetables, engage in physical activity, or sleep — due to long working hours.
So, last month, I visited the Adarsh Senior Citizen Association in New Delhi, hoping to speak with some residents about community-level obesity. The men were dressed in short-sleeved collared shirts and kurtas, with the women adorned in colorful saris — purples with henna patterns, mustards with blue flowers on stems, and oranges of Indian sages — over dusty pink trousers. Beyond the samosas and flat soda being passed around was the usual bickering — “don’t move this chair, I’m eating off of it!” or “you’re in the way, move your chair!”
With my guide Shabbir Khan, I spoke to Mangi Lal about how he was seeing obesity rapidly increase in his community, but the government was doing a little about it. Of course, the doctors had told him to eat fresh food and exercise, but Mangi Lal told me plainly that nobody in their community could really afford to do that.
Another man, Sunil Kumar, described how it’s just too hard with processed food so cheap, whether it’s the instant noodles maggi, or McDonald’s French fries (especially with those golden arches). In Sunil’s case, he’s disciplined himself to eating one roti and salad in the evening to help control his obesity but says it’s difficult because this diet leaves him weak and tired all the time. What struck me about our conversation was that Sunil doesn’t really see much malnutrition anymore.

Members of the Adarsh Senior Citizen Association with me in the top right and Shabbir Khan and some local volunteers in the bottom rowIndeed, India has been very good at addressing malnutrition, in part because the solutions are straightforward: feed the hungry. (Of course, this must be done sustainably, with focus on the newborn’s first 1000 days.) Addressing obesity, however, is much more difficult and multifactorial, with different strategies needed for prevention and treatment, as well as a radical willingness to break down the obesogenic environment. “Starvation and poverty are not a disease; it’s a state of condition you are living in,” says Baijal. “But obesity is a disease.”
India lags behind here, with limited uptake of bariatric surgery (as aforementioned), but also no Indian trials testing GLP-1 medications like Ozempic and Wegovy. This might actually matter since Indians have a “thin fat” body type, prone to high blood pressure and type 2 diabetes regardless of weight. And on average, heart disease strikes them a decade earlier with 40% increased mortality. (I described these patterns and the issue of “normal weight obesity” in an article this past May for Slate.)
And that’s not to mention that India has no food label policy, according to the Global Food Research Program at UNC-Chapel Hill — unlike over 40 other countries. This, of course, compounds on the poverty and poor health literacy in the nation. So, when Big Food companies are thinking about how to continue maximizing shareholder value, perhaps it’s not surprising that they see India as a “fantastic growth engine.”